The integrated vascular surgery residency program at the University of California, San Francisco (UCSF) is designed to provide comprehensive, integrated training including core general surgery, vascular surgery, and endovascular surgery over the course of a five-year clinical program. Consistent with our tradition of training leaders in academic vascular surgery, trainees will have 2 years of academic development time between the third and fourth clinical years, which can be spent conducting research or pursuing an advanced degree.
The integrated residency program complements our long-standing “5+2” fellowship program in Vascular and Endovascular Surgery, the first recognized vascular surgery program in the United States. The program accepts one candidate per year directly following medical school.
Clinical Training
Clinical training is obtained at four integrated sites within San Francisco, which provide a broad exposure to patient populations and healthcare systems. All of these urban clinical sites are also integrated within the UCSF general surgery residency program and they leverage the core educational infrastructure of one of the premier surgery training programs in the United States.
Clinical training includes a total of 22 months spent on core surgical rotations, and 38 months of experiences concentrated on vascular surgery that provide broad exposure to diverse patient populations and varied healthcare systems.
Research
Residents will have 2 years of funded academic development time between the third and fourth clinical years, which can be spent conducting research or pursuing an advanced degree. Faculty conduct a wide array of basic science, translational, clinical, and health services research, which involve trainees at all levels. Previous mentees of faculty members have been successful in applying for and receiving their own research funding, including competitive NIH research grants. The Division’s research is enriched by the world-class environment for inquiry at UCSF, the nation’s leading public institution in NIH funding.
Conferences, Symposia, and Education
- Vascular Surgery Grand Rounds (weekly)
- Journal Club (monthly)
- Morbidity, Mortality and Preoperative Case Conference (weekly)
- Cadaver lab (annually)
- Annual UCSF Vascular Symposium and Robert W Binkley Visiting Professorship
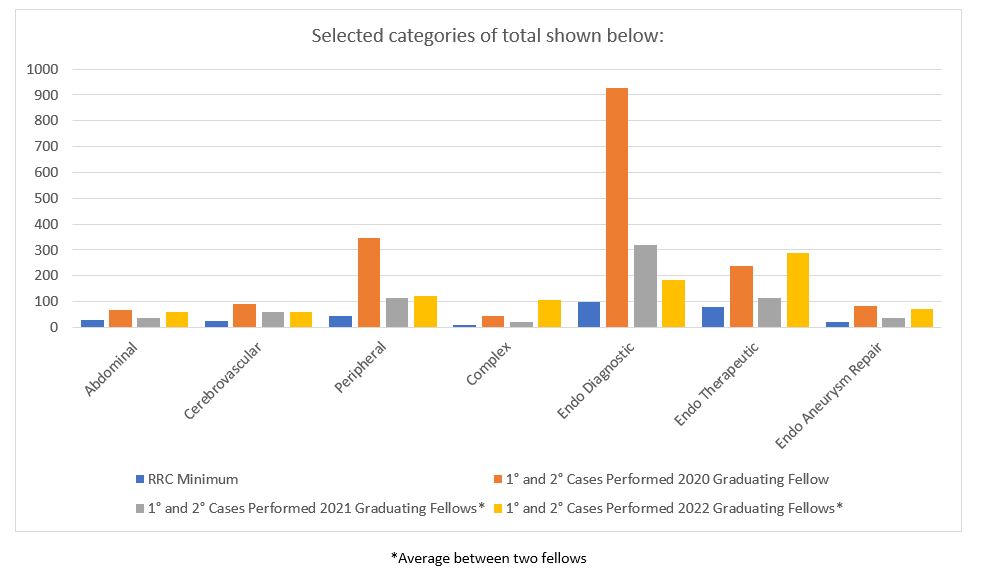
2020-2023 Graduating Fellows' Operative Experience
- Broad open and endovascular experience; high complexity
- Independent clinical research project
- 2020 Graduating Fellow = 1,374 total cases over two years
- 2021 Graduating Fellows = 775 and 568 total cases over two years
- 2022 Graduating Fellows = 1,003 and 1,031 total cases over two years
About UCSF
UCSF is one of the world’s leading medical universities and aspires to advance health worldwide. The Medical Center, consistently ranked within the top 15 in the nation by US News and World Report, occupies seven major sites in the San Francisco Bay Area. There are a total of 28 academic departments, with 8 organized research units and 5 interdisciplinary research centers.
UCSF ranks first among public institutions and second among all United States institutions in National Institutes of Health (NIH) dollars awarded. UCSF is ranked 5th by US News & World Report in the quality of research training and in the quality of primary care training, the only medical school that is ranked in the top five in both categories. UCSF is also ranked among the top 10 in all medical school specialty programs.
UCSF Department of Surgery
The UCSF Department of Surgery is one of the largest clinical services at UCSF. Surgical training programs at UCSF are among the most competitive in the nation. Additionally, the Department has a major commitment to creative activity in bench research, clinical training, education, research and global health, ranking 3rd in NIH research funding among departments of surgery nationwide. The Department’s General Surgery residency program is a premier surgical training program, which consists of 84 clinical residents and 16 research residents. The Department consists of nine divisions, which are all dedicated to providing superb patient care, conducting meaningful research, and educating the future generation of leaders in surgery.
UCSF Vascular Surgery Integrated Residency Policy on Supervision of Residents
At all sites participating in the UCSF Vascular Surgery Integrated Residency Training Program, patient care is provided by credentialed attending surgeons, either directly or through active supervision of residents enrolled in the Program. As such, the attending surgeon delegates authority to the resident, but always has the ultimate responsibility for the patient. The chain of responsibility begins with the resident and ascends to the attending. However, the chain of command does not require that the discharge of responsibility and communication of information always proceed in a step-wise manner through the patient care hierarchy. The Vascular Surgery Academic Office will maintain a published call schedule that will clearly identify the attending and resident with the primary patient care responsibility for a given time interval at each participating site in the Program. The schedule will be publicly available and made known to the resident. It will specify the contact mechanism (pager number, home phone number, cell phone number) and will be current and accurate at all times. It is expected and required that the resident contact the attending to report any new clinical circumstances, either involving an established patient or a new patient. In specific, the resident will contact the responsible attending in the following circumstances:
- Following any new consultation on an inpatient, outpatient, or emergency room patient.
- Following any telephone contact from a remote site referring physician.
- Following any telephone contact from a patient or patient family member.
- Before any admission.
- For any significant change in clinical status including transfer to ICU, hemodynamic instability, respiratory compromise, acute organ failure, acute change in mental status, change in pulse status, DNR status change, change to end of life care, or any complex patient management situation.
- Prior to performing any invasive bedside procedures.
- At any time that the patient or a family member asks that the attending be contacted. At any time the resident needs to communicate clinical information, if the attending of record is temporarily unavailable, the resident can and should immediately move to the next level in the patient care hierarchy. This means notifying the Program Director or the Division Chief. Competencies and Supervision Surgery residents are expected to master many technical procedures during their training.
All procedures are performed under supervision as well, with the nature of the supervision dictated by the clinical situation and the experience and expertise of the surgery resident. Adequate training requires the graduated assumption of increasing responsibility for patient care, including the assumption of a more primary role in the performance of operative procedures. Nonetheless, it is expected that there will be immediate attending supervision at the appropriate level for all procedures performed in the operating room. In addition all procedures performed in non-operating room settings require supervision. These guidelines for vascular resident supervision are not meant to prevent or delay the provision of emergency care during a life-threatening event. In those circumstances, clinical judgment and common sense should dictate the actions of the vascular trainee. In addition to these supervision policies, the vascular surgery resident will also function under the site specific supervision policies in place at each institution.